ALGEBRA MADE SIMPLE AT YOUR CONVENIENCE
Hire Experienced Tutors to
Ace Your Math Assignments
Crack the Code of Algebra!



Our Algebra Assignment Help Service
Welcome to our Algebra Assignment Help service!
We understand how difficult it can be to learn Algebra, especially when you have a lot of assignments to complete and no one to help you out.
That’s where we come in. We are a team of experienced math tutors who specialize in Algebra. We have helped countless students achieve their academic goals and we are ready to help you too.
Our tutors are available for hire to assist you with your Algebra assignments and projects. They have a solid understanding of the math concepts and can provide step-by-step guidance to help you solve even the most complex problems.
We guarantee that you will receive high-quality work that meets your requirements and exceeds your expectations.
Don’t let Algebra give you sleepless nights anymore. Hire our experienced tutors today and see the difference in your grades!
Only Professionals Handle the Tasks
Our tutors are highly qualified professionals who hold advanced degrees in mathematics, such as a Master’s or Doctoral degree, and have completed rigorous training in Algebra. They have a deep understanding of the mathematical principles and concepts and bring their professional experience to each tutoring session.
Our Algebra tutors have years of experience teaching Algebra to students from different academic levels. They have worked in various education settings such as schools, colleges, and universities. Thus, they have mastered the art of explaining complex mathematical concepts in simpler terms for easier comprehension by students.
Our Algebra tutors understand the importance of thoroughness in the handling of assignments. As such, they are committed to providing quality support to students. They provide guidance in problem-solving, help students create study strategies, and provide feedback on each step of the way.
Testimonials
Our Services
Our Math Tutors will gladly help you with:
Algebra Assignment Help
Our Algebra Assignment Help service is designed to assist students struggling with Algebra assignments and projects.
Mathematics Assignment Help
Our Mathematics Assignment Help service is tailored to meet the needs of students who require help with various math concepts.
Calculus Assignment Help
Calculus can be a challenging subject, but with our Calculus Assignment Help service, students can easily tackle complex assignments and projects.
Geometry Assignment Help
Our Geometry Assignment Help service is designed to assist students struggling with geometry assignments and projects.
Probability Assignment Help
Our Probability Assignment Help service is tailored to meet the needs of students who require help with probability concepts.
Trigonometry Assignment Help
Trigonometry can be a challenging subject, but with our Trigonometry Assignment Help service, students can easily tackle complex assignments and projects.
Online Math Courses/Classes Help
Our Online Math Courses/Classes Help service is designed for students who are enrolled in online math courses and classes.
How Our Service Works

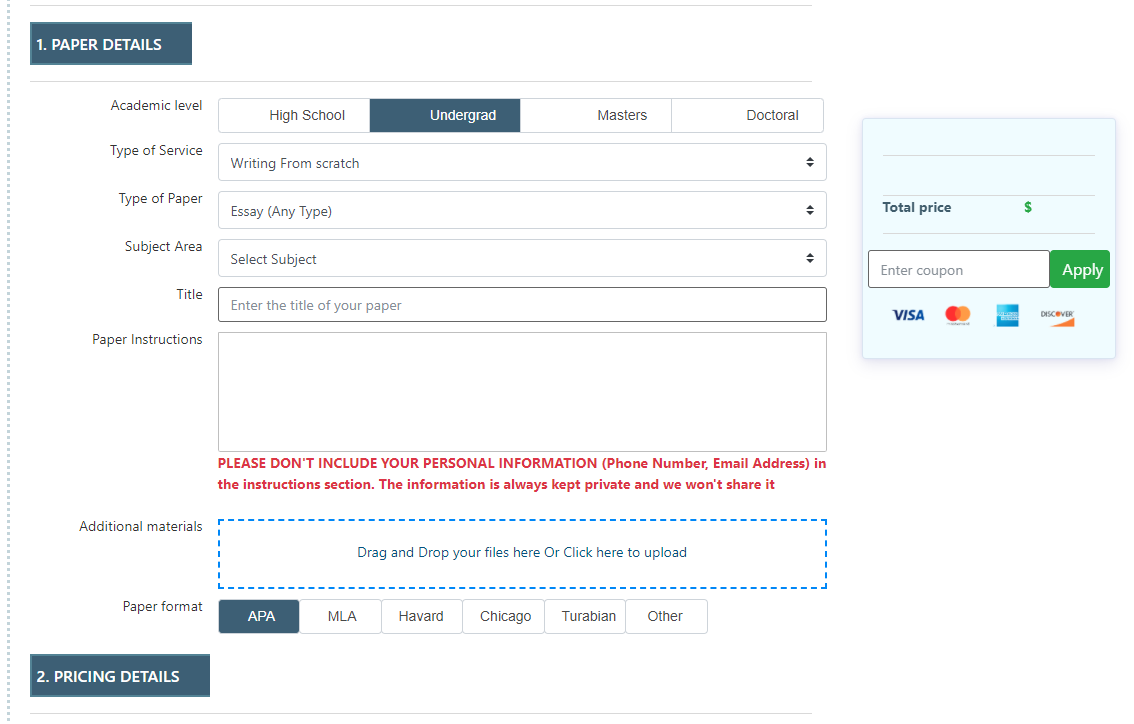
Place Your Order
Simply fill out the order form on our website, including your requirements and deadline.

Get Matched With a Tutor
We will match you with a tutor who is best suited to your needs.

Work With Your Tutor
Communicate with your tutor via our platform and receive feedback as we help you complete your assignment.

Receive Your Completed Work
We will deliver your completed work to you before the deadline.
Why Choose Our Algebra Assignment Help Service
Access to Experienced Tutors
Our website provides access to experienced tutors who are knowledgeable in the field of Algebra. With our experienced tutors, you get personalized help that is tailored to your specific needs.
Flexibility
Our tutors are flexible and can work with multiple time zones. We understand that students have busy schedules, and we make it our priority to accommodate them.
Affordable Pricing
We offer our services at affordable pricing, without compromising on the quality of work. We believe that every student deserves high-quality help, and we aim to make our services accessible to all.
Timely Delivery
We understand the importance of deadlines, and we strive to deliver all work before the deadline. With our website, you can be sure of timely delivery of your work.
24/7 Support
We understand that students may need help at any time, which is why our tutors are available around the clock to assist you.
Quality Work
Our tutors provide work that is of the highest quality. They work with you to ensure that you understand the concepts and you can apply them in solving problems on your own.
Free Features

-
$15.99Plagiarism report -
$10.91The best writer
-
$7.99Formattingreport -
$3.99Outline
-
$4.99Title page -
$21.99Unlimited Revisions
FAQs
We offer various math services, including Algebra Assignment Help, Mathematics Assignment Help, Calculus Assignment Help, Geometry Assignment Help, Probability Assignment Help, Trigonometry Assignment Help, and Online Math Courses/Classes Help.
Our tutors are highly experienced and knowledgeable in mathematics. They hold advanced degrees, and they have years of experience teaching math and helping students succeed in their coursework.
To get started, simply visit our website and fill out the order form indicating the type of service you need. Once we receive your order, we will match you with the most suitable tutor who will guide you through the process.
Our services are affordable, and the cost varies depending on the type of service you need. We offer competitive pricing without compromising on the quality of our work.
We cover various levels of math, from basic algebra to advanced calculus. Our experienced tutors are experts in various areas of math and can provide personalized support to students of all levels.
Yes, we can help you with your math homework. Our experienced tutors are available to assist students with their homework assignments and projects.
Our tutors are available 24/7, and you can communicate with them through our online platform. You can send them messages, share documents, and discuss your needs.
Yes, we are committed to delivering work before the deadline. We understand the importance of timely delivery and strive to provide timely support to all our clients.
Our tutors are highly qualified and knowledgeable in mathematics. They hold advanced degrees in mathematics and have years of experience teaching math and assisting students in their coursework.
Yes, we guarantee the confidentiality and privacy of all our client’s information. We believe in maintaining the integrity of our client’s personal information at all times.
We offer secure payment methods that are convenient for our clients. We accept various payment methods, including credit cards, debit cards, and PayPal, among others.
Yes, we allow clients to request for revisions on their work if they are not satisfied with the results. We are committed to providing high-quality services that meet our client’s needs and requirements.
Our Services
- Algebra Assignment Help
With our Algebra assignment help service, students will gain the necessary skills and confidence to tackle even the most complex Algebra problems. We provide 24/7 support to students to work around their busy schedules, and we guarantee timely delivery of all work.
Our affordable prices ensure that every student can access our high-quality services. With our Algebra Assignment Help service, students can rest easy and focus on their studies, knowing that they have expert help for all their Algebra needs.
- Calculus Assignment Help
Our experienced math tutors provide personalized guidance and support to help students develop their skills and understanding of calculus.
We cover a wide range of calculus topics such as differentiation, integration, limits, and applications of calculus. Our tutors are passionate about maths and are dedicated to helping students succeed in their calculus classes.
- Probability Assignment Help
Our experienced math tutors provide personalized guidance and support to help students develop an in-depth understanding of probability.
We cover a wide range of probability topics, including statistical inference, random variables, and probability distributions. Our tutors use real-world examples to help students apply probability concepts in problem-solving.
- Online Math Courses/Classes Help
Our tutors have a deep understanding of various online math platforms, and as such can provide step-by-step guidance on how to use each platform effectively.
With our Online Math Courses/Classes Help service, students can rest easy knowing they have expert help for all their online math needs.
- Mathematics Assignment Help
We cover a wide range of mathematical topics, including algebra, calculus, geometry, probability, and trigonometry. We help students build their confidence and develop a deep understanding of the subject.
Our tutors provide step-by-step guidance and support to help students solve even the most complex mathematical problems. Our affordable prices ensure that every student can access our high-quality services.
- Geometry Assignment Help
Assignment Help service is designed to assist students struggling with geometry assignments and projects. Our experienced math tutors provide personalized guidance and support to help students navigate through complex geometry problems.
We cover a wide range of geometry topics, including Euclidean geometry, coordinate geometry, and trigonometry. Our tutors are patient and thorough in their approach, ensuring that students have a deep understanding of the concepts.
- Trigonometry Assignment Help
Our experienced math tutors provide personalized guidance and support to help students develop their skills and understanding of trigonometry.
We cover a wide range of trigonometry topics such as trigonometric functions, identities, and equations. Our tutors are patient and thorough in their approach, ensuring that students have a deep understanding of the concepts.
